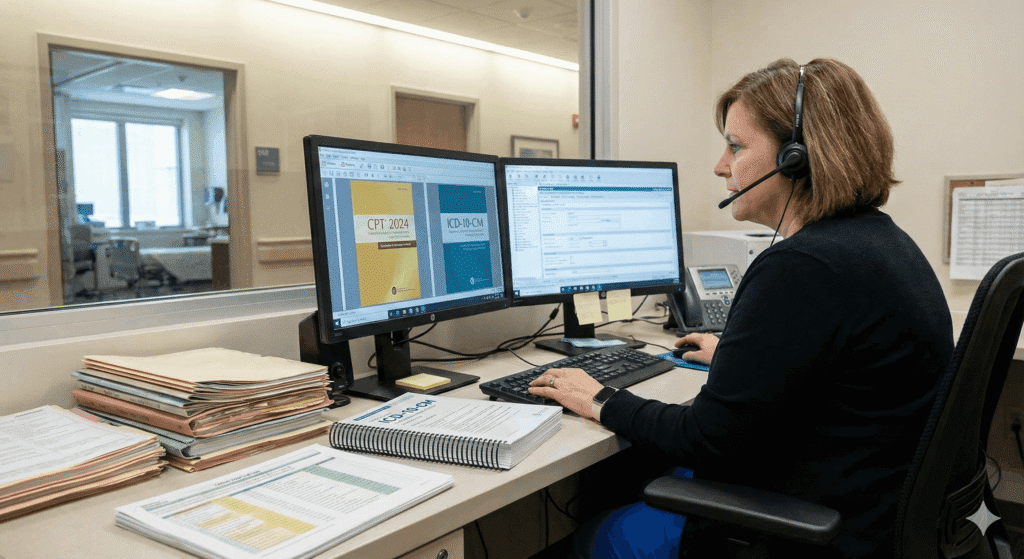
ICD-10 Codes for Cardiology: A Comprehensive Guide to Accurate Cardiovascular Coding

Introduction Cardiovascular diseases (CVDs) represent one of the most complex and highly documented areas in modern medicine. With millions of patients treated for cardiac conditions annually, the demand for accurate diagnostic classification has never been more important. In the world of medical coding, ICD-10-CM cardiology codes offer an extensive and detailed system for describing cardiovascular diagnoses with precision. Correct use of these codes impacts everything from reimbursement and treatment planning to quality reporting and risk adjustment scoring. This comprehensive guide covers the most essential ICD-10 cardiology code categories, coding rules, documentation requirements, common mistakes, and tips for accurate claim submissions. Whether you are a professional coder, biller, cardiology clinician, or health data analyst, this detailed overview will help you navigate the complexity of cardiology coding with confidence. Understanding the Structure of ICD-10 Cardiology Codes ICD-10-CM organizes cardiovascular diagnoses primarily under code range I00–I99, which represents Diseases of the Circulatory System. Since cardiovascular conditions vary widely in etiology, severity, and clinical context, ICD-10 offers a more granular approach than its ICD-9 predecessor. Key features of ICD-10 cardiology codes include: Because cardiology diagnoses often contain multiple comorbidities, accurate selection of ICD-10 codes depends on detailed documentation. =========================================== Major ICD-10 Code Categories in Cardiology =========================================== Below are the most commonly used cardiology ICD-10 categories, with detailed explanations and examples. 1. Ischemic Heart Diseases (I20–I25) Ischemic heart diseases involve reduced blood supply to the heart muscle. These are among the most frequently coded cardiac conditions. Examples: Documentation needed for accurate coding: Tip:ICD-10 requires coders to capture significantly more detail, particularly regarding the exact coronary artery affected. 2. Hypertensive Diseases (I10–I16) Hypertension is a foundational cardiovascular diagnosis and often associated with other cardiac and renal conditions. Common hypertensive codes: Documentation requirements: Tip:Coders must follow combination coding rules.Example:Hypertensive heart disease with heart failure = I11.0 + additional heart failure code (I50.xx). 3. Cardiac Arrhythmias (I47–I49) Arrhythmias are irregularities in heart rhythm and include a wide range of conduction disorders. Key arrhythmia codes: Documentation needed: Tip:ICD-10 requires coders to differentiate types of atrial fibrillation—this impacts risk scoring in value-based payment programs. 4. Heart Failure (I50.xx) Heart failure requires precise coding due to variations in severity, type, and clinical status. Examples: Each type further differentiates: Documentation must specify: Tip:Coders cannot assign heart failure type unless it is explicitly documented. 5. CVDs Related to the Brain and Circulation (I60–I69) These codes include stroke, subarachnoid hemorrhage, cerebral infarctions, and occlusion of cerebral arteries. Examples: Documentation must describe: Tip:Sequelae codes (I69) are used for chronic effects of stroke, not the acute event. 6. Venous and Lymphatic Conditions (I80–I89) Cardiology often overlaps with vascular medicine. Examples: Documentation needed: 7. Other Cardiac and Circulatory Codes Additional categories include: These reflect structural and functional heart diseases requiring precision coding. =========================================== Coding Guidelines, Best Practices & Clinical Documentation Tips =========================================== ICD-10 cardiology coding requires attention to detail, clinical insight, and adherence to compliance rules. Below are critical considerations for accurate coding. 1. Code to the Highest Level of Specificity ICD-10 requires coders to document: Example:“I25.119 – Atherosclerotic heart disease of native coronary artery with unspecified angina pectoris” This is far more specific than older coding systems. 2. Use Combination Codes When Required Cardiology ICD-10 commonly uses combination coding rules. Examples: Combination codes reduce errors and reflect clinical reality. 3. Do Not Code Uncertain Diagnoses in Outpatient Settings Unlike inpatient coding, outpatient ICD-10 rules prohibit coding: Instead, code documented symptoms: 4. Capture Relationship Between Conditions Physicians must clearly document causal links, such as: Without clear wording, coders cannot assign linked ICD-10 codes. 5. Avoid Unspecified Codes When Possible Unspecified codes (e.g., I10 or I50.9) are acceptable only when documentation lacks details. However, repeated use may trigger: Common Coding Errors in Cardiology Proper documentation and coder-clinician collaboration prevent these issues. The Importance of Accurate Cardiology Coding Accurate ICD-10 cardiology coding benefits: Cardiology is a high-risk audit area due to complex diagnoses and high reimbursement rates. Precision in coding ensures financial and clinical stability. Conclusion ICD-10 cardiology coding is more than just selecting a number—it requires deep understanding of cardiovascular disease, coding guidelines, documentation rules, and payer expectations. By mastering code ranges such as I20–I25 for ischemic heart disease, I47–I49 for arrhythmias, I50 for heart failure, and others, medical coders and providers can significantly improve claim accuracy and reduce compliance risks. With increasing emphasis on value-based care and risk adjustment scoring, precise ICD-10 documentation and coding for cardiovascular conditions is essential. Investing time in developing cardiology coding expertise not only strengthens your organization’s financial health but also contributes to better patient outcomes.
CPT Code 85025: Complete Blood Count With Automated Differential – A Detailed Clinical & Billing Guide
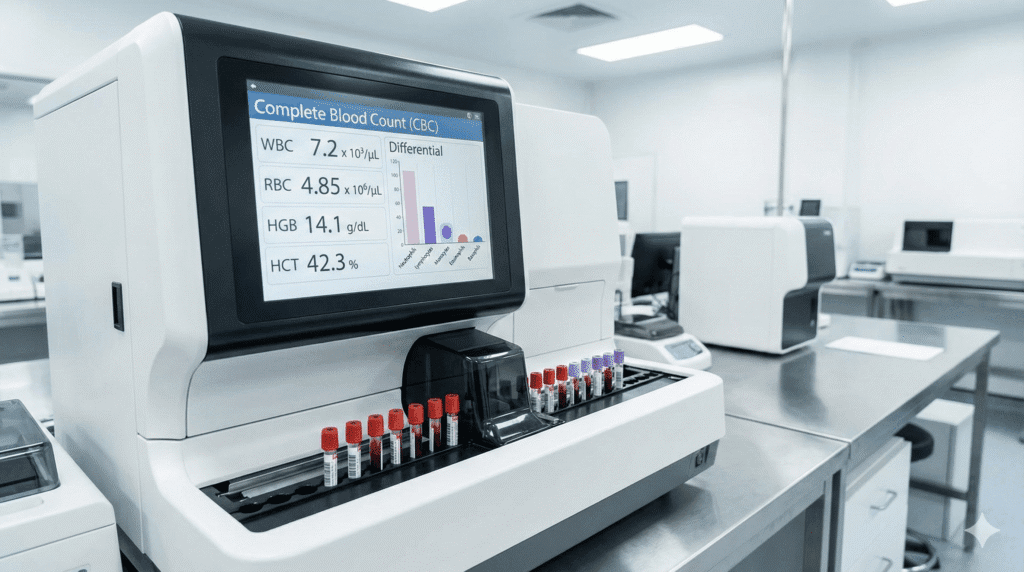
Introduction The Complete Blood Count (CBC) is one of the most essential diagnostic laboratory tests in modern healthcare. Among the multiple CPT codes used for blood count procedures, CPT 85025 is one of the most frequently billed because it represents a CBC with automated differential—a detailed lab analysis that measures multiple components of a patient’s blood. Properly understanding the clinical purpose, coding requirements, and billing considerations for CPT 85025 is critical for ensuring accurate claims submission and avoiding audit risks. This comprehensive guide explains what CPT 85025 includes, how automated differential testing works, the clinical scenarios in which it is used, and common billing pitfalls to avoid. Whether you’re a clinical provider, laboratory professional, coder, or billing specialist, this deep-dive article provides everything needed to code and bill CPT 85025 confidently What CPT 85025 Represents CPT 85025 describes a Complete Blood Count (CBC) that includes an automated differential of white blood cells. It is more detailed than a standard CBC because it analyzes both the quantity and types of different blood cells, offering more diagnostic clarity. A CBC with automated differential typically reports: These combined metrics create a detailed snapshot of a patient’s hematologic health. Understanding Automated Differential Testing Historically, differential blood counts were conducted manually by laboratory technicians using microscopy. However, modern laboratories rely on automated hematology analyzers capable of processing thousands of samples per hour. Key advantages of automated differential testing include: Automated differentials also allow clinicians to detect subtle hematologic abnormalities, such as early infections, immune dysregulation, or bone marrow disorders. Clinical Scenarios Where CPT 85025 Is Used A CBC with differential is one of the most frequently ordered laboratory tests across nearly all medical specialties. Providers rely on it for diagnosing, monitoring, and managing a wide range of conditions. 1. Infection and Inflammation WBC levels and differential patterns help identify: 2. Anemia and Nutritional Disorders Red blood cell indices aid diagnosis of: 3. Hematologic and Oncologic Diseases CBC results help screen for: 4. Monitoring Chronic Conditions Providers monitor blood trends for: 5. Preoperative Evaluations Surgeons frequently order CBCs to evaluate: The wide clinical relevance of this test explains why CPT 85025 is so widely used. Documentation Requirements for CPT 85025 Although laboratory codes typically rely on results, proper documentation is still required for billing compliance. Required documentation should include: Payers often require clear justification, especially for repetitive testing. Billing and Coding Guidelines Correct use of CPT 85025 requires understanding reimbursement rules, payer policies, and bundling limitations. 1. Do Not Bill 85025 With Certain Bundled Panels Medicare and commercial payers often bundle CBCs into broader laboratory panels.For example: Always check National Correct Coding Initiative (NCCI) edits before submitting claims. 2. Only Bill When Automated Differential Is Completed If the laboratory performs CBC WITHOUT differential, the correct code is 85027, not 85025. Many claim denials occur because: 3. Understand When Manual Differential Codes Apply If the automated analyzer flags abnormalities that require manual review, additional CPT codes may apply, such as: However, billing for both automated (85025) and manual differential is generally not allowed unless clinically justified and supported with documentation. 4. Know the Medicare Frequency Limitations Some payers limit how often a CBC with diff can be billed for a single patient per day or per week. Excessive testing must be medically justified. Examples: Documenting “frequent monitoring needed due to clinical instability” is key. Common Billing Errors to Avoid 1. Missing or Invalid Diagnosis Codes Payers often deny CBC claims when submitted with: Use diagnosis codes that clearly support the medical necessity of the CBC. 2. Billing 85025 When Only a CBC Was Performed If no differential was completed, billing 85025 is incorrect and may trigger audits. 3. Lack of Proper Physician Orders Even if the test was completed, missing documentation of the order can result in denial. 4. Repeating CBCs Too Frequently Without Justification Especially in outpatient settings, payers may classify this as overutilization. Best Practices for Compliance and Clean Billing 1. Ensure the Lab Analyzer Completes the Differential Before billing 85025, confirm the machine generated: 2. Use Diagnosis Codes That Match Clinical Context Examples: 3. Document Trends When Ordering Multiple CBCs Explain reasons such as: 4. Integrate Automated Reporting Into the EHR This improves accuracy and traceability. Why CPT 85025 Matters to Healthcare Organizations 1. Supports Accurate Diagnostic Decisions CBC with differential is foundational to detecting a wide range of conditions. 2. Ensures Reimbursement Integrity Proper coding helps avoid: 3. Improves Quality Measures Early diagnosis allows for better patient outcomes. 4. Provides Insight for Preventive Care CBC trends can detect chronic disease early. Conclusion CPT 85025 plays a vital role in clinical diagnostics and laboratory billing. As one of the most frequently performed tests in healthcare, it requires precise coding and clear documentation. By understanding what the code represents, ensuring accurate ordering, respecting payer policies, and avoiding common billing errors, healthcare organizations can maximize reimbursement accuracy and maintain compliance. A strong grasp of CPT 85025 ensures that clinicians receive timely results, labs remain compliant, and patients benefit from reliable diagnostic data that supports their treatment plans.
CPT Code 90792 – Psychiatric Diagnostic Evaluation: A Complete Guide for Providers
Introduction Accurate medical coding is fundamental to behavioral health reimbursement, clinical documentation integrity, and regulatory compliance. Among the most frequently used codes in psychiatric and mental health settings is CPT 90792, the code for Psychiatric Diagnostic Evaluation With Medical Services. Providers who deliver diagnostic evaluations that include medical elements—such as reviewing labs, conducting physical exams, managing medications, or assessing medical comorbidities—must understand the correct use of 90792 to avoid denials and ensure clinical clarity. This extended guide provides a deep exploration of CPT 90792, covering what the service includes, how it differs from CPT 90791, necessary documentation requirements, payer expectations, and frequently misunderstood billing scenarios. Whether you’re a psychiatrist, psychiatric nurse practitioner, or a billing professional supporting behavioral health, this article provides the detail needed for consistent and compliant use of CPT 90792. What CPT 90792 Represents CPT 90792 describes a comprehensive psychiatric diagnostic evaluation that includes medical services. This distinguishes it from 90791, which is used by non-medical clinicians or by situations where medical components are not performed. The service typically includes: 1. A Thorough Psychiatric Assessment This includes: Psychiatrists are expected to document mental status examinations and patient interactions in detail. 2. Medical Evaluation Components Since 90792 is a medical diagnostic code, the evaluation may include: These medical components justify billing 90792 instead of 90791. 3. Development of Initial Treatment Plan Providers typically outline: The treatment plan demonstrates medical decision-making, which insurers often scrutinize. 90792 vs. 90791 – Understanding the Difference Confusion between these two codes is common. The distinction matters because using the wrong code may cause denials or compliance issues. 90791 – Non-Medical Diagnostic Evaluation Used by: This code does not include medical evaluations, prescribing authority, or physical examination. 90792 – Medical Diagnostic Evaluation Used by: This code requires medical decision-making and medical assessment. Key Reminder:If any medical component is performed, even a medication review or ordering labs, 90792 is generally the correct code. Required Documentation for CPT 90792 Payers expect documentation that supports the comprehensive nature of the evaluation. Thorough documentation protects against audits, improves care quality, and justifies reimbursement. 1. Patient History Include: 2. Mental Status Examination (MSE) A complete MSE typically covers: 3. Risk Assessment Evaluate for: 4. Medical Components This is essential for 90792. Examples include: 5. Diagnostic Formulation Providers should include: 6. Treatment Plan This is critical for demonstrating clinical decision-making: When 90792 Can Be Billed 1. Initial Patient Evaluation 90792 is most commonly billed for a patient’s first psychiatric appointment. 2. Re-Evaluation After Extended Time It may also be billed again when: 3. Telehealth (Modifier 95) 90792 is frequently used in telemedicine with Modifier 95 when permitted by payers. Documentation must clearly indicate: 4. Coordinated Care Cases If the provider must review extensive medical records or collaborate with other clinicians, this code is appropriate. Common Billing Mistakes to Avoid 1. Billing 90792 Without Medical Components If no medical services are provided, payers may deny the claim because it should have been billed as 90791. 2. Copy-and-Paste Documentation Auditors look for: 3. Failing to Document Medical Necessity Examples of strong documentation: 4. Using 90792 for Medication-Only Visits 90792 is for diagnostic evaluation, not routine follow-ups. Medication management follow-ups require E/M coding (e.g., 99214). Best Practices for Providers 1. Use Structured Templates Providers who use structured templates often produce more complete documentation. 2. Clarify the Medical Components Explicitly state activities such as: 3. Align Documentation With Complexity If the patient presents with multiple comorbidities, explain how these affect psychiatric care. 4. Explain Time Spent (If Required by Payer) While CPT 90792 is not time-based, insurers may request clarification when audits occur. Conclusion CPT 90792 is an essential code for psychiatric providers who conduct comprehensive, medically informed evaluations. Proper documentation, understanding of medical components, and a structured approach to assessment ensure clean claims, enhance payer compliance, and improve patient outcomes. As behavioral health expands, accurate use of 90792 becomes foundational for clinical and financial success.

